The term osteochondrosis itself is derived from two words: osteo - bone and chondru - cartilage. Put simply, it is an ossification of cartilage. Although this interpretation is fundamentally wrong. Some go further in their delusions and believe that osteochondrosis is the build-up of salts in the joints. It is also table salt that is said to be consumed in large quantities for food.
Pathogenesis
In reality, everything works a little differently. And harder. And table salt, if it plays a role in the occurrence of osteochondrosis, is very indirect. Osteochondrosis is due to degeneration and degeneration of the articular cartilage. This is not a disease in its own right, but a pathological process that can be observed almost anywhere where there is connective cartilage tissue.
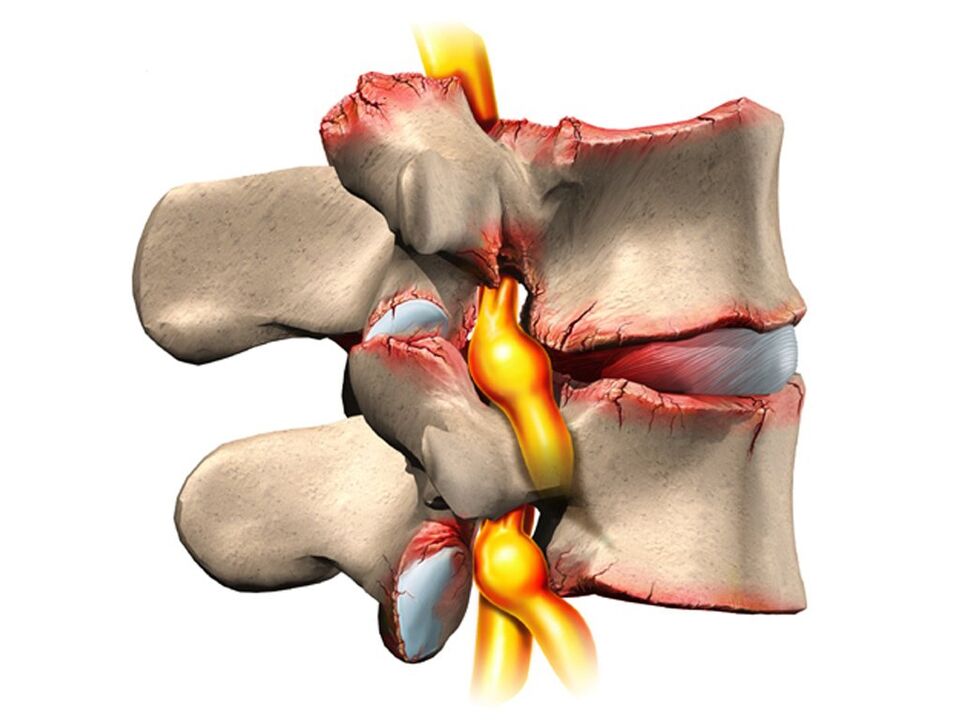
Still, osteochondrosis overwhelmingly affects the spine. Why so? The fact is that between the vertebrae there is a kind of cushion - intervertebral discs (intervertebral discs). The physiological task of these intervertebral discs is to cushion the vertebral bodies and to protect them from premature wear due to mechanical stress. The intervertebral disc consists of an inner liquid nucleus pulposus, which is surrounded by an annulus fibrosus and an upper and lower endplate.
The intervertebral disc is subject to enormous mechanical stress, which leads to permanent damage to its structures at the cellular level. In humans, these processes are too pronounced - this is our payment for walking upright. To prevent the disk from being completely "erased", it must constantly regenerate, ie rebuild. It is the balance of damage regeneration processes that determines the normal structure of the intervertebral disc. Another curious detail is that the intervertebral discs are not supplied with blood and nutrients via the blood vessels that have grown together in childhood, but diffusely from the bone tissue of the vertebral bodies. Again, paying for the ability to move on two limbs, not four.
As a result, the intervertebral discs are easily injured in anatomical and physiological terms. Every negative process in the body leads to an imbalance in the damage-regeneration balance and to the development of dystrophy and degeneration of the intervertebral discs. A structurally defective pane can no longer withstand the correct mechanical stress. Under excessive pressure from the vertebrae above, the intervertebral discs are shifted in different directions, usually to the side and back. This process is known as a herniated disc.
The bone tissue of the vertebrae that has lost its cartilage lining is also subject to mechanical wear. Due to constant trauma on the anterior edge surface of the vertebral bodies, pathological bone growths - osteophytes - are formed. Spondylosis develops. Due to degeneration and dislocation of the intervertebral disc, the intervertebral spaces shrink, the spinal canal narrows and the roots of the spinal nerves in the so-called foramina foramina are injured.
causes
The causes or etiological factors of osteochondrosis are diverse. They can be both local, that is, due to the pathology of the spine itself, and general disorders at the level of the organism. Any pathology that leads to a violation of the structure of the spine or metabolic disorders can be considered the cause of osteochondrosis. In this regard there are:
- Changes in the configuration of the spine (scoliosis, pathological lordosis or kyphosis).
- Other defects of the musculoskeletal system are flat feet, a narrow shoulder girdle, abnormalities in the pelvic structure.
- Spinal injury.
- Weak immunity.
- Metabolic disorders - osteoporosis, obesity, diabetes mellitus, thyroid disease.
- Diseases of the cardiovascular system - atherosclerosis, hypertension.
- Digestive disorders resulting in insufficient absorption of nutrients from the gastrointestinal tract.
- Inheritance.
It should be noted that the above pathological conditions do not necessarily lead to osteochondrosis. This requires constant exposure to certain predisposing factors - hypothermia, malnutrition, sedentary lifestyle or, on the contrary, excessive physical exertion.
Symptoms
Osteochondrosis itself is an asymptomatic process. At the same time, the signs of intervertebral disc degeneration are diverse. How come? The fact is that the clinical manifestations of osteochondrosis are due to its complications - disc hernias, spondylosis, sciatica, narrowing of the spinal canal.
In addition, the clinic is very variable depending on the prevailing localization of the process in the cervical, thoracic or lumbar spine. The last section is most commonly affected as the lower back receives maximum physical activity. Signs of osteochondrosis of the lumbosacral region:
- Pain (lumbodynia, lumbago, sciatica).
- Restriction of movement of the lower back and the lower extremities (intermittent claudication).
- Here sensory disorders of the type of paresthesia appear - numbness, burning, creeping.
- Pathological tension of the lumbar muscles.
- Without treatment, functional disorders of the pelvic organs.
Cervical osteochondrosis is observed somewhat less often than lumbosacral. However, this pathology is also quite common. In addition to the typical pain symptoms (cervicalgia), reduced sensitivity and movements in the upper extremities, cervical osteochondrosis has its own characteristics due to impaired blood flow to the brain. These properties manifest themselves:
- Insomnia.
- Headache, dizziness.
- Periodic nausea.
- General weakness, easy fatigue.
- Fluctuations in blood pressure.
- Occasionally toothache.
- Behavioral reactions in the form of tears, irritability.
The chest area with osteochondrosis is relatively rarely affected. Patients in this case are people who are professionally forced to sit in a stable uncomfortable position - students, schoolchildren, programmers, office workers. The symptoms of osteochondrosis in this case are as follows:
- Chest pain and paresthesia.
- Dyspnea.
- Feeling of heartbeat.
- Restricted movement of the thoracic spine.
diagnosis
From all of this, it becomes clear that osteochondrosis is a chameleon disease. Due to the similarity of signs, it is easy to confuse it with cerebrovascular accident, hypertension, myocardial infarction, angina, neurotic disorders. Therefore, in order to make the correct diagnosis, a comprehensive complex diagnosis is required in order to correctly determine the symptoms and treatment of osteochondrosis.
In addition to the classic questioning and clarification of patient complaints, this diagnosis should include a medical examination and special examination methods. These methods include x-ray of the spine, ultrasound of the internal organs. Recently, computed tomography and magnetic resonance imaging have been used successfully to diagnose osteochondrosis.
treatment
Therapeutic tactics for osteochondrosis include the use of:
- Medication.
- Massage.
- Physiotherapeutic procedures.
- Physiotherapy (exercise therapy).
- Manual therapy.
- Acupuncture.
Medicines for osteochondrosis are mainly aimed at relieving pain and eliminating inflammatory processes in the nerve roots. In various combinations, these drugs are often used in the form of ointments, injections and tablets for the treatment of osteochondrosis. It should not be forgotten that these drugs have a negative effect on the liver, stomach and intestines. As a result, they can aggravate metabolic disorders in osteochondrosis. They relieve the pain of the blockage well with local anesthetics. The effect of these agents is short-lived and in no way affects the course of osteochondrosis as a whole.
With the help of drugs such as chondroprotectors, immunostimulants and vitamins with minerals, it is possible to improve metabolic processes at the local and body level. Chondroprotectors are used in tablets, ointments and ampoules. Among the tonics, vitamin C, group B, is used in combination with minerals. In this regard, calcium supplements are most preferred. In fact, contrary to some erroneous claims, osteochondrosis is not based on an excess, but merely a lack of calcium.
After successfully relieving the exacerbation, physiotherapeutic procedures, massage and exercise therapy are shown. The physical methods used are electrophoresis with calcium, phonophoresis with hydrocortisone, amplipuls, paraffin therapy. All of these measures are aimed at eliminating pain and inflammation in the nerve roots, ligaments and muscles. Massage for osteochondrosis is carried out according to the generally accepted method. The massage zone is selected depending on the location of the osteochondrosis. The expansion of the range of motion is achieved with the help of exercise therapy. At the beginning, in the exacerbation phase, there are practically no dynamic loads. The patient is always in an optimal posture. At this time, it is desirable to wear immobilization devices - a lumbar corset, Shants' neck collar. As the exacerbation subsides, the volume and duration of movements during exercise therapy increases.
Recently, in the treatment of osteochondrosis, non-traditional methods of treatment have been used - acupuncture, manual therapy, osteopathy. Acupuncture is an effect on specific biologically active points along the spine, on the auricles, on the hands and on the feet. In manual therapy, the normal position of the vertebrae and intervertebral discs is restored through the manual action of a specialist's hands. And in the course of osteopathy, targeted techniques ensure the structural integrity of the musculoskeletal system. In the absence of the effect of conservative measures to treat osteochondrosis, persistent pain, complications, surgery is indicated. The pathologically displaced intervertebral disc is removed. A microdiscectomy is currently being performed for this purpose - endoscopic removal of a displaced intervertebral disc.

















































